What is Masticatory Muscle Myositis in Dogs?
Masticatory Muscle Myositis is an autoimmune disease or process where the immune system targets the masticatory muscle (a large muscle in the jaw). Dogs suffering from this disease will often present in the clinic with jaw pain, lack of eating, or a complete inability to even open their jaw!
However, what is up and down with this sometimes overlooked disease? Take a read below and learn more about the issues with this canine masticatory muscle myositis!
Pathogenesis of Canine Masticatory Muscle Myositis
Antibodies are continuously circulating in the blood system. They are part of a very beneficial immune system that protects our dogs (and us) from pathogens (basically anything that can cause diseases).
Sometimes, however, mistakes can happen within our immune system, which causes autoimmune diseases. For example, Masticatory Muscle Myositis is an inflammatory myopathy (muscle disease) caused by an autoimmune process where the body starts attacking the big masticatory muscle placed in the dog’s jaw.
Why exactly this happens is unknown. One theory is that T-cells (a type of antibody) respond to a pathogen (e.g., a bacteria), but at the same time, it also cross-reacts with the body itself. It is a complicated process, but it can lead to autoimmune diseases, like this, where the T-cells/antibodies start attacking the body itself!
What exactly causes this cross-reaction is challenging to say. Some dogs are more predisposed to autoimmune reactions, and many different agents can then trigger the diseases. From viral and bacterial exposures to vaccinations, hormones, and stress! Most of the time, the vet will not pinpoint the exact trigger that started the autoimmune disease.
Nonetheless, once the disease has been triggered, the immune system will attack the muscle tissue in the jaw, and only the jaw as this is the only place in the body with the particular 2M muscle fibers. As these are only in the jaw, this is why symptoms are only seen here and not anywhere else in the body.
The Signs of Masticatory Muscle Myositis in Dogs
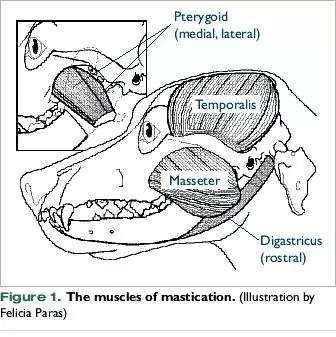
Masticatory muscles are found on the sides of the head, and these muscles are primarily involved in chewing. When the muscles get attacked by the immune system, it causes the muscles in the jaw to become swollen and painful.
The swelling and pain lead to the symptom most often associated with masticatory muscle myositis: The inability to open their mouth–at least not without experiencing excruciating pain.
The inability to open will lead to other secondary symptoms that include lack of eating, stop picking up their toys, and general severe pain and discomfort. In some dogs, one can even visualize the swelling on the outside of the jaw. The jaw might even look smaller in some dogs due to having atrophied (been broken down).
Dogs may also display ophthalmic (eye) signs in the early stages of the disease; these include:
- Protrusion of the third eyelid
- Red eyes
- Exophthalmos (when the eye is bulging out of the socket)
Most dogs are around three years of age at the onset of disease, but it can occur at any age, with some reports of patients being as young as four months old. So, if the dog starts displaying any of these symptoms, it is crucial to give your local veterinarian a call as soon as possible!
Which Dog Breeds Are Predisposed to MMM?
It is important to remember that Masticatory Muscle Myositis can occur in any breed and gender. However, some dog breeds are genetically more predisposed to developing autoimmune reactions, including Masticatory muscle myositis. These breeds include:
- Golden Retrievers
- Cavalier King Charles Spaniels
- Dobermans
- German Shepherds
- Weimaraners

Just because a dog breed is predisposed to developing genetic diseases does not mean it will automatically develop Masticatory Muscle Myositis or something similar. It is just essential to keep in mind if your dog ever starts displaying some of the symptoms mentioned above–and knowing when to consult a veterinarian.
How is Masticatory Muscle Myositis in Dogs Diagnosed?
Masticatory muscle myositis can become a pretty severe and complicated disease, which tends to worsen over time. Eventually, muscle fibers can be completely gone, and muscle fibrosis occurs, which leads to irreversible jaw dysfunction. Therefore, early and accurate diagnosis is essential!
When a dog presents in the clinic with a swollen or sore jaw, inability or reluctance to chew, and perhaps a history of eating less, a complete physical and neurological examination is necessary. This is to determine whether the signs are related to the jaw muscles exclusively or if anything else might be affecting the dog.
If it is determined that the issue originates solely from the jaw, a definitive diagnosis is made with a 2M antibody test. The antibody test detects the specific antibodies that attack and destroys the muscle fibers (called 2M fibers) in the jaw.
Besides the 2M antibody test, a blood chemistry test should also be done to determine the creatine kinase (CK) level in the blood, which may be elevated due to muscle damage as the disease progresses over time.
Other diagnostic tests may also be employed to rule out or confirm a suspected diagnosis of Masticatory muscle myositis.
False negatives are possible (where it is wrongly decided that a dog does NOT suffer from a particular disease). False-negative diagnosis can happen in cases where a dog has been given significant doses of immunosuppressive medication for seven to ten days before the antibody test is done. This is why it is imperative to tell your veterinarian about any medication or supplement your dog may be receiving!
However, it is essential to remember that Masticatory Muscle Myositis is a pretty rare disease, and not everything that causes jaw pain will be this. Other causes of jaw pain in dogs can be:
- Tetanus
- Muscular dystrophy
- Foreign body in the mouth
In these cases, the 2M antibody test will be negative, which is why this test is the gold standard for diagnosis of Masticatory Muscle Myositis and is what a veterinarian will determine treatment off.
Available Treatment Options Against MMM
In the end, the most important thing for owners(and veterinarians)–is to recognize the problem as early as possible, as this is vital to help a dog regain its ability to open its jaw pain-free.
Corticosteroids (like prednisolone) are often the cornerstone of therapy during the acute phase, as these are aggressive immunosuppressive drugs. Corticosteroids will inhibit the antibodies attacking the 2M muscle fibers and allow the muscles to recover.
A high dosage of corticosteroids should be continued until a dog regains complete jaw function and the creatinine kinase levels are expected once again. After this, the dosage can be lowered as long as clinical symptoms are controlled.
Some dogs may be able to discontinue the corticosteroid treatment altogether, but most will need lifelong therapy with a maintenance dosage. In addition, most dogs will experience relapse quickly if treatment is discontinued too soon or too much.
Unfortunately, as wonderful as corticosteroids can be, they do come with some side effects that are essential to be aware of and control. Some of these are:
- Excessive urination
- Excessive drinking
- Excessive appetite (and weight gain)
Prognosis of Masticatory Muscle Myositis in Dogs
The prognosis is generally good for dogs with Masticatory muscle myositis, but it can vary quite a lot, with early diagnosis and prompt treatment being the most critical factors. Dogs that receive aggressive corticosteroid treatment during the acute phase generally have a good outcome.
However, if the disease has not been diagnosed correctly or too late, scar tissue will start forming in the jaw muscle, which can cause permanent issues.
Even with an excellent initial prognosis, many dogs will, unfortunately, relapse, with relapses often being harder to treat and a worsening prognosis following suit. Therefore, a forecast will generally need to be given for each dog based on clinical signs, degree of fibrosis, and how well a dog will respond to the corticosteroid treatment.
A prognosis can also be determined by taking a muscle biopsy (a small sample of tissue from the muscles). With this, a veterinarian will determine the degree of muscle fiber destruction and any other pathological changes there may be present and thereby give as accurate a prognosis as possible.
Remember, however, that even in the best of cases, a prognosis is an educated guess. Some dogs may surprise and have a better response to therapy, whereas others may worsen faster than we would want to wish for.
FAQ’s on Canine MMM For Veterinarians
Q: What do I need for the 2M antibody assay/test?
A serum (blood) sample of 1-2 ml. A fasting sample is recommended, but the assay/test has not been shown to be affected by hemolysis (the breaking up of red blood cells) or lipemia (the presence of fat) unless severe.
Q: What is the 2M antibody assay, and what is its sensitivity and specificity?
The 2M antibody assay is an enzyme-linked immunosorbent assay (ELISA). Small plastic wells are coated with masticatory muscle myositis antigens, where serum from a dog suspected to suffer from MMM is placed on top.
If the dog has any 2M antibodies present in the blood, these will attach to the antigens in the wells. Often a color-bonded enzyme will then be added to the solution to determine the presence of antibodies by displaying a color. The absorbance (intensity of the color) is then measured. A higher intensity meaning more antibodies present.
Sensitivity or “true positive” (simplified) means how good the test is to determine whether a patient is carrying the disease. If sensitivity is very high – as it is with ELISA – the test will be very good at defining a true positive carrier of the disease as actually being positive.
On the other hand, specificity is a measurement of how good a test determines that a patient does NOT have the disease. High specificity means that it is infrequent for an ELISA test to miss a positive. Conversely, if the test is negative, the patient is almost certainly not carrying the disease.
Q: Do I need a muscle biopsy and the 2M assay for a diagnosis?
Ideally, it would be best if you did both. The 2M antibody assay will provide the definitive diagnosis – remember to cease any corticosteroid treatment before the test. If the 2M antibody test is positive, the dog is suffering from Masticatory muscle myositis.
The 2M assay, however, does not provide any information about myofiber destruction or fibrosis there may be present, which are very important when determining a prognosis. Owners are likely to want to know the diagnosis and whether the return of jaw function and muscle mass is a possibility to determine the best course of action.
Q: What other conditions can look like Masticatory muscle myositis?
During the clinical exam, the most apparent sign of masticatory muscle myositis is the atrophy (breaking down) of the jaw muscle, often bilaterally. However, this atrophy can also occur after long periods of corticosteroid therapy and should therefore not be mistaken as masticatory muscle myositis.
Disorders in the temporomandibular joints (the jaw joints) should also be ruled out. This will most often be done with x-rays that can determine any possible bone changes.
Atrophy of the jaw muscles could also be caused by polymyositis, a chronic inflammatory disease in the muscles. Similar to masticatory muscle myositis. However, this will affect several (or all) muscles in the body and not the 2M muscle fibers in the jaw solely.
Q: What is the treatment for Masticatory muscle myositis?
(Note: Do not attempt to treat Masticatory muscle myositis yourself. Treatment should always be decided and overseen by a qualified veterinarian).
When a correct diagnosis has been made, immunosuppressive doses of corticosteroids should be started. Generally, the recommended dosage is 2mg/kg/day until normal jaw motion has returned and the Creatinine Kinase levels in the blood are normal.
Hereafter the dosage of corticosteroids can be gradually decreased until dosage has been reached where a dog is still experiencing no clinical signs. Remember to see the dog frequently for check-ups to control any recurrences of clinical symptoms and educate owners to look out for symptoms of flare-ups.
